Welcome to the online version of our Trust strategy 2025-2030. The content on this page was taken from our strategy document, created in June 2025. To navigate between chapters, please use the buttons at the bottom of this page. Alternatively, if you would like to view the full document, please download a copy here.
Chapter four: our strategic aims 2025-2030
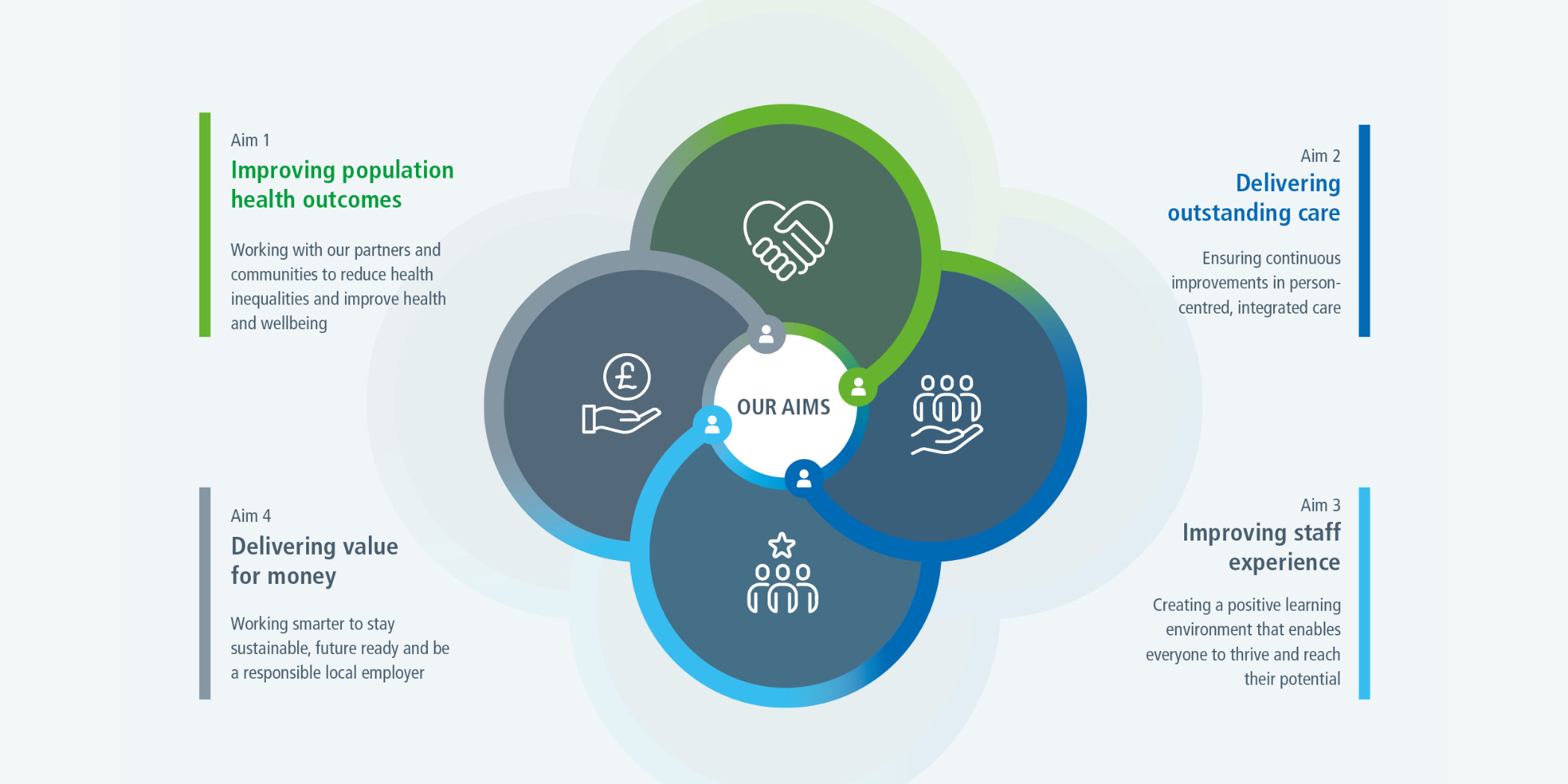
It is clear from our data, national and local priorities and what people told us, that we need to strengthen our focus on health outcomes, deliver outstanding care, support our workforce and work more efficiently and effectively together. To do this we have based our strategic priorities on four key aims; a widely adopted framework that evidence suggests works well to support fair and effective healthcare models and improve overall community health.
Data and evidence
Available data and evidence about access, outcomes, inequalities, demographics and population health (our strategic needs assessment).
National and local priorities
Analysis of current and future strategic and policy context and national NHS and local partner strategies and research evidence on best practice.
Feedback we received
Themes from engagement and co-design work with colleagues, patients and service users, their families and carers, our communities and partners.
Our strategic aims
Aim 1: Improving population health outcomes
Working with our partners and communities to reduce health inequalities and improve health and wellbeing
Aim 2: Delivering outstanding care
Ensuring continuous improvements in person-centred, integrated care
Aim 3: Improving staff experience
Creating a positive learning environment that enables everyone to thrive and reach their potential
Aim 4: Delivering value for money
Working smarter to stay sustainable, future ready and be a responsible local employer
We have split each of our four aims into three strategic goals, to ensure a focused, structured approach that translates our ambitions into clear, actionable steps, driving measurable progress and impact.
| Our strategic goals |
|---|
| Better outcomes - we will support people of all ages by focusing on their overall health and wellbeing taking a more preventative approach to help improve health at every stage of life. |
| Fairer health - we will work proactively with all our communities to improve access, experience and outcomes with an enhanced focus on priority groups. |
| Co-production - we will improve collaboration and work together with our communities and partners and ensure people with lived experience are at the heart of all we do. |
-
We will use data and evidence to target support earlier, coordinate care for those who need it most, and deliver joined-up services that improve health and reduce crises across all ages.
-
We will work collaboratively with partners including GPs, local authorities, and local communities to improve population health including wider social determinants.
-
We will make ‘every contact count’ (Physical health with Mental Health) to support healthier behaviours, better well-being and create better connectivity and community empowerment.
-
We will lead on the development with partners of enhanced crisis care pathways to reduce the severity of cases and the number of people needing emergency support.
-
We will have demonstrable evidence from staff, service users and communities on the progress to becoming an Anti-Racist Trust and delivery of the patient and Carer Race Equality Framework (PCREF plan).
-
Our service users and patients will report that reasonable adjustments are consistently met when accessing services without them having to repeat their needs. Services will be digitally inclusive, and language will not be a barrier to accessing care in a timely way.
-
All physical health checks for; children and young people, people with serious mental illness and learning disabilities, will support connections with positive intervention to improve health and wellbeing.
-
We will work closely with system partners and the ICB to enable children to receive the best start to life and receive care and support as early as possible to enable better outcomes and a successful transition to adulthood.
-
Culture change in which co-production and the voice of lived experience is embedded in all we do including in our collaboration with community partners.
-
Increased capacity of our lived experience workforce and providing them with consistent and high-quality wellbeing support, supervision and development, with career progression.
-
Our understanding of experience of care is fundamental to strategic, operational, improvement and transformation decision making.
- Detailed population needs reports will have been produced by all 7 divisions of the Trust identifying proactive and preventative services for their population.
- There will be 50% less duplicate contacts across mental health and physical health services.
- There will be a 5-10% reduction in physical and mental health crisis presentations.
- There will be improved physical health outcomes for patients in our mental health and learning disability services.
- Year on year reduction in the excess mortality rate in adults under 75 between 2027-2030.
- No significant variance in access, experience or outcome measures for priority groups across our all-age services.
- Fewer people in Hampshire and Isle of Wight will die by suicide.
- The total number of people with serious mental illness and learning disability who have meaningful occupation will be higher in 2030.
- No inequity in access, experience and outcomes for Black and Asian patients detailed under the Mental Health Act.
- By March 2027 the number of children in HIOW receiving both a 12-month health review and a 2-2.5-year health review will either be at or exceed national average percentages.
- Co-production and lived experience leadership infrastructure is in place.
- Increased number of people employed in lived experience roles to a minimum of 10 per 100,000 of the registered population by year 3.
- Evidence of lived experience membership and attendance in all Trust-wide and Divisional governance meetings.
- Evidence of experience, employment support and development of lived experience workforce.
- Evidence of co-production in all improvement training, including an increase in peer trainers.
- 95% of recruitment panels to have lived experience representation and involvement in the interview process.
Patient feedback:
“I want equal access to services.”
| Our strategic goals |
|---|
| Person-centred care - we will deliver compassionate, empathetic, personalised care. |
| Joined-up care - we will work with partners to enable joined-up pathways of care that are easy to navigate. |
| Continously improving - we will embrace research, learning and continuous improvement to deliver outstanding care. |
- Improved safety, experience and clinical outcomes, with people using services, their families and staff reporting feeling more supported by the trust and their reasonable adjustments met.
- We will enable neurodivergent young people and their families to access earlier support ahead of diagnosis.
- A shift from hospital to community care through the delivery of neighbourhood models and closer integration of physical and mental health interventions. Providing right care, right place, right time, right professional to improve flow through healthcare services.
- Less avoidable ambulance conveyances and inappropriate admissions to inpatient beds with patients cared for in the most appropriate setting.
- Enhanced flow and coordinated discharge for all mental health service users.
- Embedded referral management system and process based upon continuous learning and population needs which optimises and reduces all waiting times across HIOW.
- Evidence of a learning and continuously improving organisation demonstrated by staff survey results, lived experience input and improvement in outcomes.
- By March 2027 all the Delivery of Culture of Care standards will be implemented with the Quality Committee providing assurance on their impact.
- Year on year improvement in patient engagement and experience scores.
- There will be a 5-10% reduction in physical and mental health crisis presentations.
- Reduce average length of stay in adult mental health beds by 15% by March 2026.
- Increase access to crisis alternatives to improve flow and reduce 12-hour breaches in A&E by 50% by 2027.
- Reduced length of stay in community rehabilitation beds to national average including a reduction in patients with no criteria to reside to 12.5%.
- Reduce out of area placements to zero by March 2027 and maintain at this level.
- Deliver a 10% improvement in waiting times to access Child and Adolescent Mental Health Services (CAMHS).
- By March 2026 publish report detailing the implementation of the learning directly related to the Nottinghamshire Homicide Review.
- Deliver a single community model for Urgent Community Response and virtual wards which delivers 85% occupancy (a 5% improvement on the national target).
- By March 2026 achieve national planned care targets and:
- Reliable improvement target of 68% within Talking Therapies.
- Reliable recovery target of 50% within Talking Therapies.
- Less than 10% of people waiting more than 90 days between 1st and 2nd appointment within Talking Therapies.
- Reduction in patients waiting over 52 weeks on Children and Young People’s community waiting lists.
- Reduction in the number of patients waiting between 18-51 weeks on community waiting lists.
Patient feedback:
“I want to be involved in decisions about my care.”
| Our strategic goals |
|---|
| Positive learning culture - we will have a positive, well-led collaborative culture across our organisation. |
| A thriving workforce - we will create an environment where our staff excel; feel safe, supported, valued and engaged. |
| Effective staff development - we will support every person to reach their potential. |
- Trust CARE values are fully embedded, delivered through Living our Values programme.
- Our leaders will be visible and engaging, demonstrating Leading with CARE.
- Our people will recognise there is no tolerance of discrimination of any kind.
- Strengthened professional networks and enhanced specialist support.
- We will be a learning organisation, characterised by strong research and improvement capability and clear evidence of effective services that innovate and continously improve.
- Our people feel safe, well and healthy with the processes, programmes and management support that meet their needs.
- A co-owned staff engagement programme to address the issues that impact on the ability to thrive at work.
- All staff and students are offered comprehensive career and skills development and career pathways.
- A learning and development offer enables a learning culture where all staff reflect, learn and develop.
- From March 2027 our compassionate culture score in the NHS staff survey will improve year on year and be consistently above sector average benchmarks.
- By 2030 we will maintain Good CQC Well-led rating.
- Year-on-year quantifiable improvement against national workforce race and disability equality standards.
- By March 2026, we will have an integrated improvement plan in every clinical division.
- By March 2027, we will have a co-designed suite of measures demonstrating effectiveness with linked programmes of improvement.
- From March 2027 our NHS staff survey overall engagement will improve year-on-year and be consistently above sector average benchmarks.
- A year-on-year reduction of workplace aggression incidents is reported.
- By 2030 we will have evidence of a sustained reduction in turnover.
- A year-on-year reduction in overall staff sickness rates based upon 2025 rates.
- From April 2026 we will have yearly improved scores in NHS staff survey ‘We are always learning’ measures.
- By 2030 improved attraction and retention of those in early careers and critical healthcare roles.
| Our strategic goals |
|---|
| Financial sustainability - we will improve productivity and efficiency and meet our financial obligations. |
| Optimised resources - we will maximise use of our infrastructure (estates and digital) enabling our operational and transformation priorities. |
| Key local employer - we will act as an anchor institution demonstrating environmental, social and corporate responsibility including a new Green Plan. |
- Greater sustainability of clinical services.
- Improved productivity and efficiency of clinical and support services.
- Reduced unwarranted variation in corporate service benchmarking.
- Buildings and facilities that are fit for purpose and well utilised by our staff and communities.
- Our workforce are enabled to work in an agile way supporting the effective delivery of their roles.
- New Digital solutions implemented to increase productivity and impact.
- Recognised as an anchor institution with demonstrable evidence of impact upon our communities across Hampshire and the Isle of Wight.
- Successful delivery of NHS Net Zero target.
- Successful delivery of a balanced financial revenue plan every year to 2030.
- Annually deliver a comprehensive set of capital bids against relevant priorities with a success rate of £3m year on year from 2025.
- Ensure minimum cash levels of at least 10 operating days.
- A demonstrable year-on-year improvement on the underlying £31m deficit position from 2025.
- Reduction in cost and numbers of agency staff by 30% by end of 2025/26.
- Reduced spend on support functions with the aim of achieving lower quartile to median against sector benchmarking.
- Demonstrable year on year improvement against targets within productivity dashboard.
- Reduction in the cost of bank staff by 10% by end of 2025/26.
- All temporary staff to be less than 0.5% of pay bill by 2030.
- By 2030 the Trust to remain in the mid to lower quartile of the national Estates Return Information Collection (ERIC) when benchmarked against peers - demonstrating efficient and effective use of estate.
- Maintain then improve year-on-year NHS Staff Survey results for staff perceptions of having adequate materials, supplies and equipment to do their work.
- Year-on-year improvement in our NHS Digital Maturity Assessment score.
- Releasing more clinician time to care and reducing the time patients wait to access care.
- A year-on-year reduction in clinician time spent on administrative tasks through use of Artificial Intelligence (AI) tools.
- By March 2026 we will have successfully undertaken an assessment against the UCL partners Anchor model (or similar) and co-designed clear measurable board approved baseline targets.
- We will be on track to meet Net Zero for carbon emissions we directly control by 2040.
Staff feedback:
“I want seamless IT systems and buildings that are fit for purpose.”
We will collaborate with our partners to deliver our four strategic aims and implementing the changes and improvements needed across all of our adult and children and young people’s services, as well as our supporting corporate services.
We will also prioritise a number of specific transformation programmes each year, focused on delivery and real impact – shaped by the feedback we have received.
In 2025/26 we will focus our efforts on the following transformation programmes:
- Frailty
- Integrated Neighbourhood Models
- Adult Mental Health
In addition, we will work to deliver the Children’s Partnership Board priority of giving children the best start in life during the first 1,001 days.
- A single email and file sharing system
- Review our Electronic Patient Records
- Financial recovery
All enabled by our new CARE values and Organisational Development Plan.
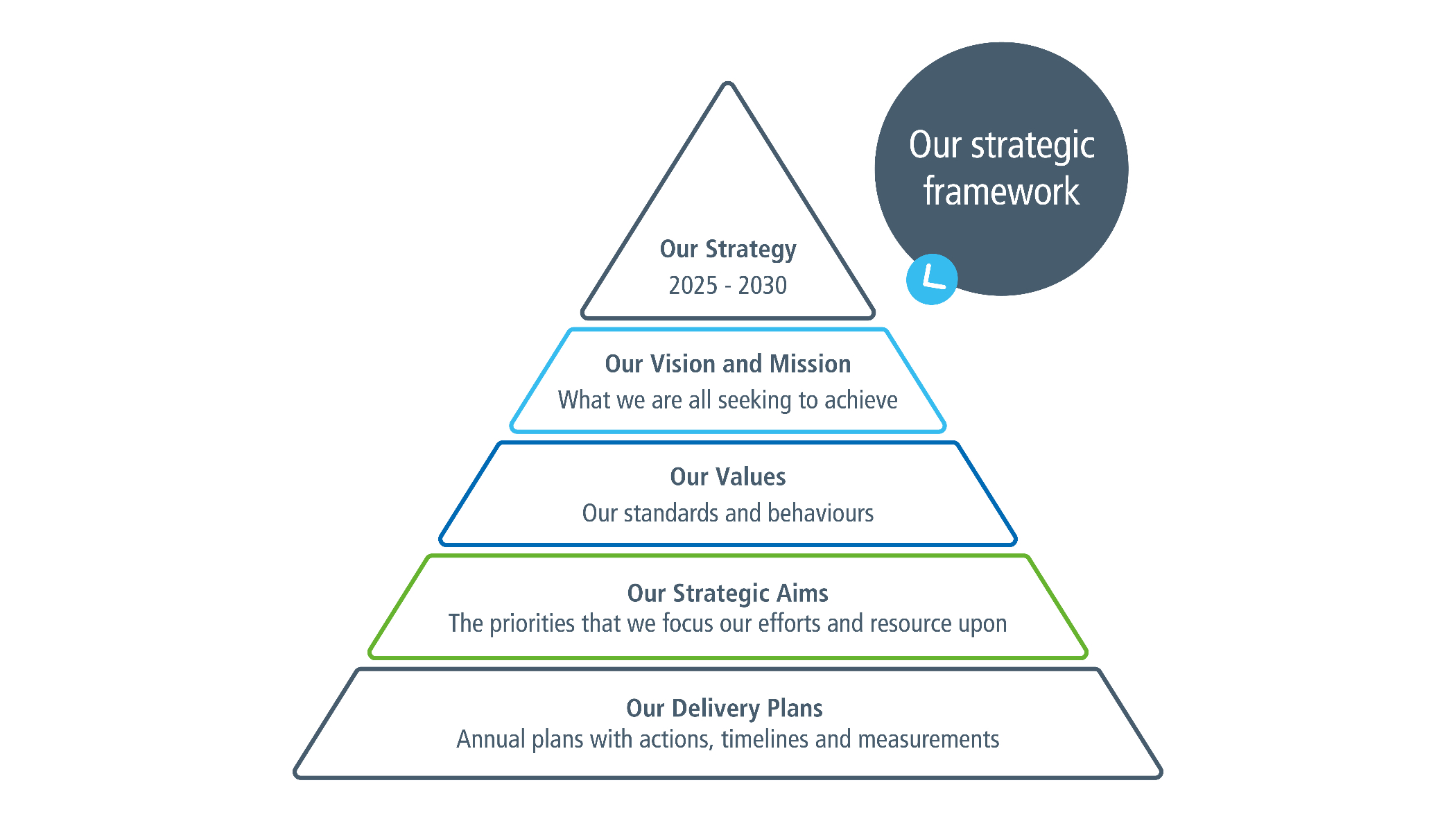
Our strategic framework
- Our strategy 2025 - 2030
- Our vision and mission - what we are all seeking to achieve
- Our values - our standards and behaviours
- Our strategic aims - the priorities that we focus our efforts and resource upon
- Our delivery plans - annual plans with actions, timelines and measurements
Achieving what truly matters most to people will only be possible by working together.
By continuing to collaborate, share knowledge and develop solutions alongside our valued partners, we can make sure our improvements really make a sustainable difference to people and communities.
We are very grateful to all our partners who have been involved in the development of this strategy and look forward to working with them to turn these plans into action.

- Regulators
- Carers and families
- Community partners
- Local employers
- Voluntary sector
- Politicians (national and local)
- Healthwatch
- Social care providers
- Local authorities
- Patients and service users
- Hampshire and Isle of Wight Healthcare NHS Foundation Trust
- Academic partners
- Police, crime and justice
- Fire and rescue
- All health services
- Education
- Anchor Institution - an organisation that has a significant stake in a local community and a large presence in the local area.
-
Anti-Racist - an advocate for racial justice, actively identifying and opposing racism.
-
Care Pathways - a structured guide that outlines the care process for a specific condition or procedure.
-
Community rehab beds - beds for short-term stays in the community, particularly after a stay in hospital.
-
Co-production - a collaborative approach where individuals or groups work together, sharing power and responsibility to design, develop and deliver services, products or projects.
-
Culture of Care Standards - NHS guidance for providers of inpatient mental healthcare.
-
Digitally inclusive - everyone regardless of background or abilities has equal access to and the skills to use digital technologies effectively.
-
Green Plan - A plan for how we will minimise our environmental impact to deliver the NHS-wide ambition to reach net zero carbon emissions by 2040.
-
HIOW - Hampshire and Isle of Wight.
-
Lived Experience - personal, direct, first-hand knowledge and understanding gained through living through an event, situation or condition.
-
Neighbourhood Models - different ways of organising and delivering services within a geographical area.
-
Net Zero - the balance between the amount of greenhouse gases (carbon) produced and going into the atmosphere and those that are removed from the atmosphere.
-
NHS Digital Maturity Assessment - a self-assessment tool that allows an organisation to determine their readiness to respond to changes and trends in technology.
-
No criteria to reside - when a patient is medically fit to leave and should be discharged.
-
Nottinghamshire Homicide Review - an independent mental health homicide report into the homicides in Nottinghamshire.
-
Person centred care - care tailored to the needs, preferences and values of an individual.
-
Quality Committee - the Quality Committee provides assurance to the Board of Directors on the quality of care provided to the Trust’s patients.
-
Social determinants - the non-medical factors that influence a person’s health and wellbeing (for example education, economic stability).
-
Talking Therapies - psychological treatments that involve talking with a trained professional about your thoughts, feelings and behaviours.
-
UCL Partners Anchor Model - a toolkit providing guidance and support to local health anchor institutions.
-
Unwarranted variation - differences in care delivery that cannot be explained by patient need, illness or evidence based guidelines.
-
Virtual ward - provides hospital level care to patients in their own homes using technology for monitoring and treatment.