The Trust is managed via the Board who are responsible for performance and provide the strategic direction to ensure we deliver high quality, safe services.
The Board is made up of:
- Executive Directors - responsible in their executive role for managing the organisation and, as board members, for the leadership and direction of the Trust.
- Non-Executive Directors who do not have a managerial role but are responsible for challenging the Executive Directors in decision-making and on the Trust’s strategy.
Collectively they are responsible for our overall performance and our plans for the future.
We also have a Council of Governors comprising elected staff and public Governors, as well as appointed Governors. Our Governors represent the views of Foundation Trust Members drawn from our local population. Governors help the Trust make decisions about our services and hold our Non-Executive Directors to account.
Our clinical services
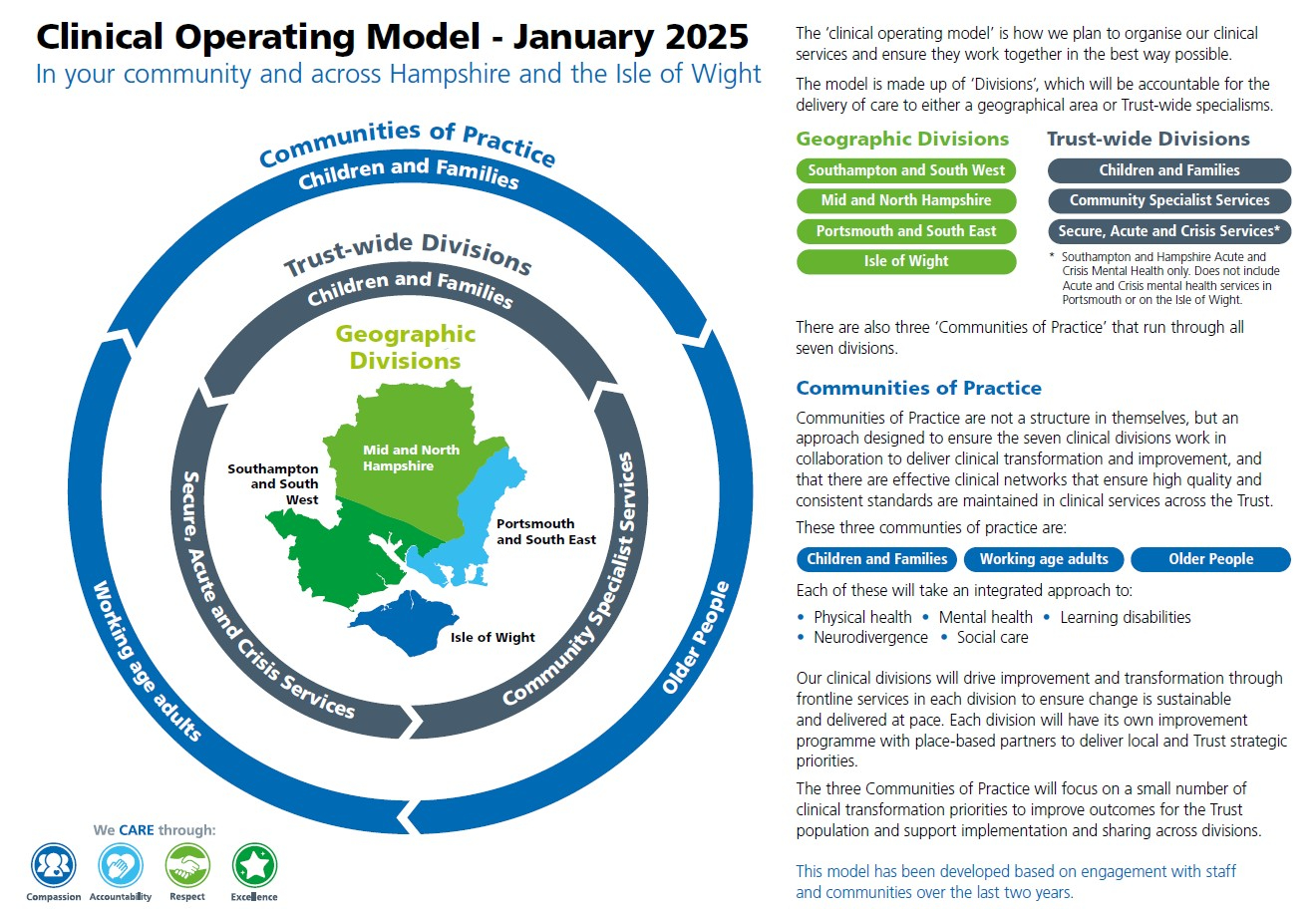
Click here to view a diagram of our clinical operating model or view it towards the bottom of this page.
Open the accordions below to read more about each element of the clinical operating model.
The clinical operating model for Hampshire and Isle of Wight Healthcare consists of 7 Divisions which group, organise and operate all frontline healthcare services. Four geographical divisions and three specialist Trust-wide ones:
- Isle of Wight Services
- Portsmouth and South East Hampshire Services
- Southampton and South West Hampshire Services
- Mid and North Hampshire Services
- Children and Families Services
- Community Specialist Services
- Secure, Acute and Crisis Services.
The 7 Divisions replace the previous 13 Divisions and services lines we had in our legacy Trusts. Importantly, there will be no disruption or change to the way front line care is delivered as the Trust transitions to this new divisional structure.
In addition to the 7 Divisions, the Trust will also have 3 ‘Communities of Practice’ to enable clinicians to work together across divisions - to share best practice, continuously improve services and meet consistent standards.
These Communities of Practice are not a structure, they are ways for staff to collaborate. Linked to every stage of a patient's life, the 3 Communities of Practice (covering both mental and physical health) are: Children and Young People, Working Age Adults, and Older People.
Using a model of ‘Connected Leadership’, our 3 Communities of Practice will enable us to work across internal organisational boundaries, learning to constructively challenge in order to continually improve, and developing trusted relationships with people who use our services (their families and carers) and system partners – all in the interests of our patients.
In addition to our 3 Communities of Practice, we will also have a number of ‘Clinical Networks’ to help connect and support clinical staff - for example: networks for Talking Therapies, CYP secure services, Neighbourhood Development, Learning Disabilities and Neurodiversity.
Ultimately, our goals as a new harmonised NHS Trust are to:
- provide integrated mental health, physical health and social care that meets the complex needs of our patients (throughout their lives), all informed by robust data.
- take a prevention and early intervention approach to all our services, to improve outcomes for patients and reduce health inequalities.
- reduce unwarranted variation, while enabling warranted variation in response to local need.
- provide clinically and financially sustainable services.
To learn more about the services we offer, visit our A-Z of services. You can also visit our ‘main sites and locations’ page to explore some of the locations we operate out of.